RESEARCH FOR A HEALTHY START TO LIFE
Mission
Empower creative thinkers to solve great challenges in development, maternal and child health.
To solve these challenges we must:
Question differently: reframe problems and data; use systems thinking; invite perceptions; trust intuition; check our certitude
Stretch to progress: create safe conditions for exploration; take risks; execute carefully and with urgency; be agile; reflect often; learn from discomfort; integrate rather than compartmentalise
Create value: generate knowledge that is valuable; commit to effective, multimodal communication for science and society; inspire people to act
and develop these traits in others.
Explore
“Business cannot prosper in a society where the potential and talents of the future generation are denied at birth”
— Prof James Heckman, Nobel laureate economist
Environment
Optimal growth and development in the first 2000 days of life from conception contributes to the immediate survival of the newborn, establishes a strong immune system in the infant, supports brain development and function, and promotes a healthy metabolism. The environments experienced by a mother before, during, and after pregnancy can shape the health of that pregnancy and the lifelong health of the mother. These same environments are also experienced by the fetus in the womb and the child after birth, and can therefore shape a child’s growth and lifelong immune, metabolic, and brain health.
Statistics
-

Obesity
Over 30% of Canadian women of reproductive age are overweight or have obesity.
Globally, 42 million children under the age of 5 are overweight and over 20% of children in Canada are overweight or have obesity.
-
Malnutrition
Undernutrition and hidden hunger remain global burdens. In Canada, 1 in 8 households experience food insecurity.
More than 1/3 of child deaths and 11% of total disease burden world wide are due to maternal and child undernutrition.
-

Preterm Birth
Maternal underweight, obesity and inflammatory conditions are also risk factors for preterm birth and low birthweight babies. Preterm birth affects 8-12% of all pregnancies.
Having low birthweight babies, early deliveries, and C-sections increases newborn care costs in Canada nearly 150 times.
In Canada, obesity and its comorbidities, including type 2 diabetes, result in a $4.6-7.1 billion annual financial burden to the Canadian economy. Despite that these diseases are preventable, only a small proportion of Canada's health care spending is dedicated to prevention.
DOHaD
Research in the field of Developmental Origins of Health and Disease (DOHaD) aims to understand how experiences during development shape disease risk and resiliency throughout the lifecourse.
Risk Factors
A risk factor is any attribute or exposure that alters an individual’s chances of developing a disease. Some of the key risk factors for preterm birth, poor growth in early life, and metabolic diseases in later life include:
-

Poverty
-

Malnutrition
-

Stress
-

Infections
-

Genetics
But not everyone who is exposed to these factors will be born too early, or grow poorly, or get diseases in later life. Interactions between the environment and the individual are critical for determining who is vulnerable and who is protected or resilient.

The Challenge
Despite incredible advances in biomedical sciences, critical aspects of female biology, maternal and pregnancy health, and fetal and child development, remain unclear. This means we have limited ability to predict health trajectories at an early stage, to enrich for resiliency and prevent adverse health outcomes.
Additionally, the increased incidence of non-communicable diseases (NCDs) later in life raises questions about the origins of these disorders and the factors operating in early life that influence development around the time of conception, in the womb, and after birth.
To prevent suboptimal development in early life and poor health across the lifecycle, we need to understand how early experiences set the developmental path of the child.
We also need new and timely interventions to modify risk factors and optimise early environments.
Solving these challenges requires us to integrate multiple systems, methods, disciplines and partnerships.
Research
Our research uses a systems approach to understand the pathways that lead to poor maternal health, suboptimal development, and chronic disease risk, and to optimise development and health across the lifecycle.
We investigate interactions between the environment, the host, and its resident microbes, using animal models and human cohorts. We aim to understand how suboptimal environments including poor nutrition and maternal disease states shape the pregnancy and risk for adverse pregnancy outcomes. We also aim to understand how these environments impact development of the placenta and fetus (particularly the gut and brain) and the growth of the infant postnatally, resetting the metabolic, endocrine, and immune mechanisms that contribute to chronic disease.
Our research is dedicated to developing:
• novel ways to predict individuals at-risk for adverse pregnancy outcomes, suboptimal development, and later chronic disease
• novel interventions to optimise maternal health and early developmental trajectories, and reduce the incidence of non-communicable diseases.
Our work aligns with international and national priorities
-
Our work aligns with the goals to “ensure responsive, inclusive, participatory and representative decision-making at all levels” and promote inclusive societies
-
Our work tackles malnutrition (including anaemia), food insecurity, child growth, and the needs of girls and pregnant people, and aims to enhance coherence and collaboration in nutrition interventions
-
Our work aims to understand outcomes including maternal and child mortality and morbidities (including congenital anomalies), reproductive health, communicable and non-communicable diseases, and the risk and protective factors underlying these
-
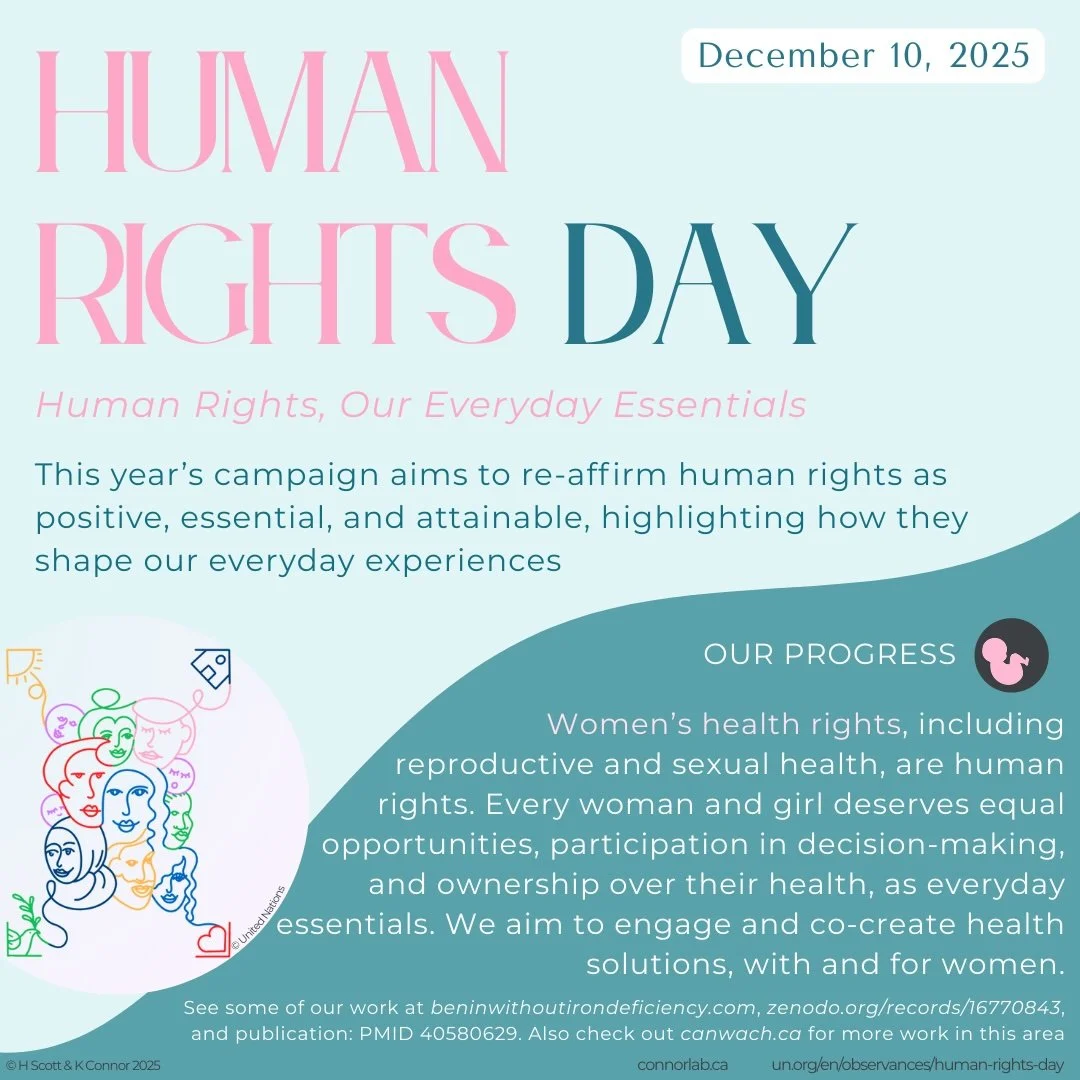
Our work strives to ensure women’s empowerment and their “full and effective participation and equal opportunities” in decision making and their health
Priorities from: United Nations Sustainable Development Goals Report 2019 & Global Affairs Canada 2018 & 2023 Agendas for Implementing the Sustainable Development Goals
Our research is transdisciplinary and translational
-
We explore our questions at many levels: from genes, to cells, organs, organisms, and populations
-
We apply diverse methods and in new ways, and are adaptive with our approaches — from ‘omics’ to cell biology, to animal models, human cohorts and trials, to data science and machine learning, through to stakeholder engagement and knowledge mobilisation
-
We have expertise in many disciplines, and prioritise integrating ideas and findings across disciplines
-
We empower, coordinate, mobilise and collaborate with diverse partners in the lab, locally, nationally and globally, including scientists, clinicians, people with lived experience, social enterprises, non-governmental organisations, governments, and the public
Our efforts move evidence towards implementation
Pipeline to impact
-
We use a systems approach in our discovery science projects:
Maternal malnutrition and metabolic state
Micronutrient deficiencies
Gut microbiome, function, and interactions with health
Viral infection in pregnancy
Placental development and function
Fetal-infant development, neural tube defects, and associated risk factors
-
We collaborate with clinicians, industry & communities in our clinical research
There is an urgent need to find novel solutions to complement and extend existing approaches for preventing and treating micronutrient deficiencies and poor metabolic health in women
We are testing novel interventions and new applications of existing therapeutics to address these health challenges
Our projects:
At-home fortification for the prevention and treatment of iron deficiency
Probiotics to improve nutrient status and gut health
Probiotics to improve metabolic disease in pregnancy
-
We engage experts by experience and use co-design approaches
Our partners: Community members, government, NGOs, industry, scientists, and clinicians
Our projects:
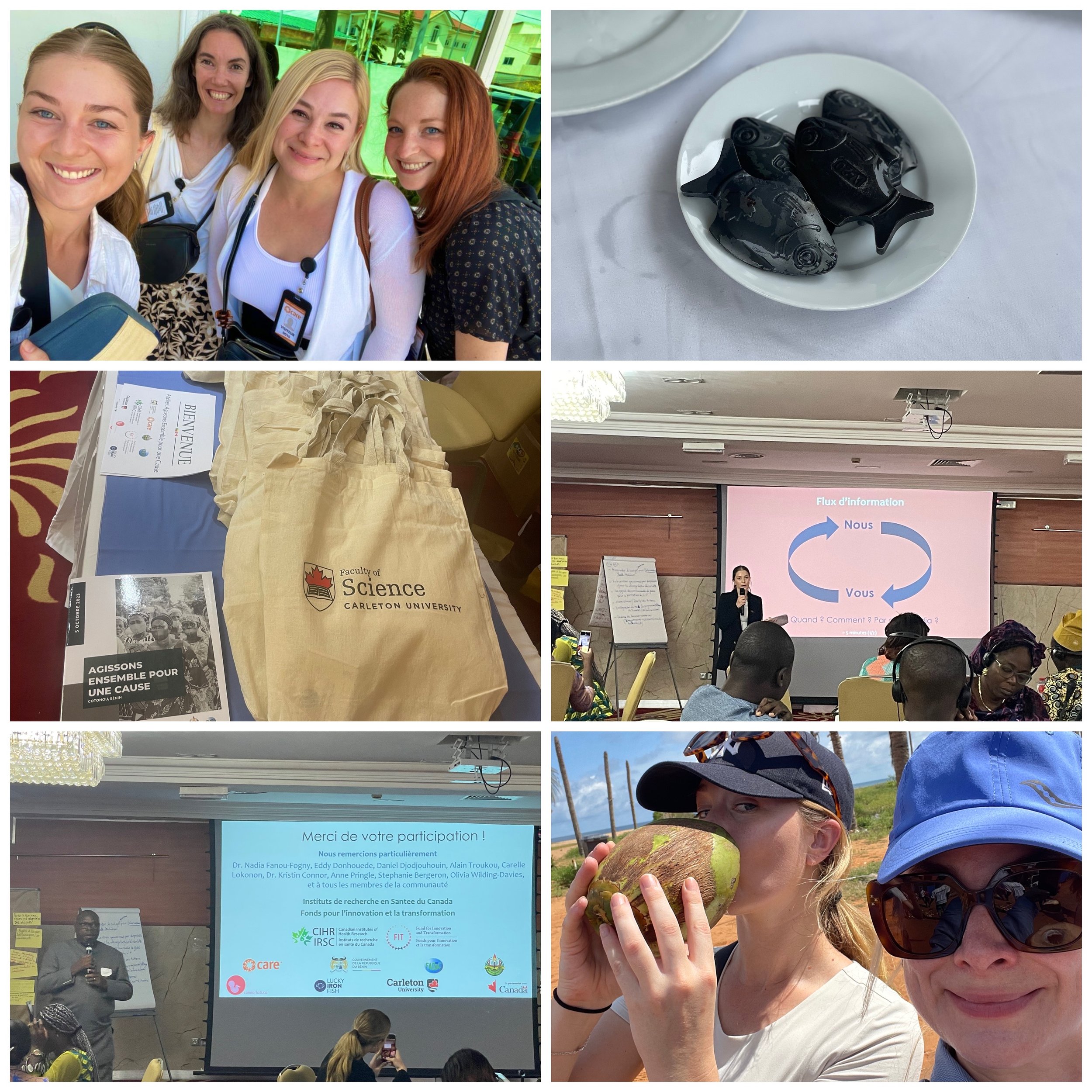
Adapting and scaling interventions to reduce iron deficiency and improve women’s and family health in Benin
Building libraries of lived experience as resources for health decision making, intervention design, and health advocacy related to: 1. preconception, perinatal, and maternal health, and 2. iron deficiency and women’s nutrition
Our capacity building:
-
We synthesise and mobilise knowledge to inspire action on women’s and children’s health
Our projects:
Evidence to close the funding gap in women’s health research and affect policy for the health of women and children
Evidence on gaps and opportunities in maternal health services for Indigenous peoples to inform better culturally sensitive healthcare
Evidence on lived/living experience to advocate for better maternal and child health care, access, and policymaking
-

Maternal malnutrition, metabolic state, and placental defence and transport
Maternal malnutrition (under- and overnutrition) and suboptimal metabolic status can induce changes in the metabolic, hormonal and immune systems in the body. If these changes target intrauterine tissues (the placenta and fetal membranes), they may hinder the ability of these tissues to protect against microbes commonly associated with the onset of preterm labour and other adverse pregnancy outcomes. These changes may also alter the transport of nutrients and other molecules to the fetus that are critical for its development. We are investigating how maternal malnutrition and metabolic and pro-inflammatory states influence placental defence and transport. These studies are part of our larger goals to understand how early life environments influence risk for preterm birth and suboptimal feto-placental development, and to develop nutrition-focused and microbe-targeting interventions to prevent these adverse outcomes and improve maternal-child health.
-

Gut development and function in response to maternal adversity
Gut bacteria have been linked to human health and disease states including obesity and diabetes, and can shape our response to the foods we eat or the medications we consume. We are investigating how common adverse conditions before and during pregnancy (maternal malnutrition, underweight and obesity, and infection) impact the integrity of the maternal and offspring intestinal barriers and the composition and function of their gut microbiomes, and how these conditions may impair the maternal-fetal interface. We are also testing novel microbe-based and microbiome-targeted interventions to improve pregnancy health and fetoplacental development. These studies are part of our larger goal to understand how the gut plays a role in coordinating exogenous signals from our environment (nutrition), and endogenous signals in our bodies (pro-inflammatory and metabolic factors), to influence maternal health and increase vulnerability to poor growth and metabolic diseases in offspring.
-

Early life environments and neural tube defects
Disruptions in fundamental developmental processes, such as cell growth and proliferation, can result from inadequate nutrient supply, leading to congenital anomalies. Neural tube defects (NTDs), such as fetal spina bifida, remain amongst the most common congenital anomalies. Specific nutrients, including B vitamins, play a critical role in the formation of the neural tube and are also essential for the high rates of DNA synthesis and cell proliferation that accompany periods of rapid fetoplacental growth and development. A key contributor to healthy nutrient levels is the gut microbiome. A healthy microbiome also supports nutrient absorption and produces other molecules that may influence placental function and nutrient delivery to the fetus. We are investigating the role of the maternal gut microbiome in the development of fetal spina bifida and its comorbidities, including poor placental development and function. These studies are part of our larger goals to understand how inadequate supply, uptake, transport and/or metabolism of key nutrients from the mother to the developing embryo/fetus may contribute to the pathogenesis of NTDs and increase risk of placental maldevelopment and dysfunction, fetal growth restriction, and preterm birth.
-

Early interventions to improve nutrition and women’s and infants’ health
Globally, mineral and micronutrient deficiencies are common in children and in women in their reproductive years, including during pregnancy. Inadequate nutrition is predictive of suboptimal lifelong health and profoundly influences development and health trajectories in the next generation. Given the intergenerational cycle of nutrient deficiencies, there is a window of opportunity to replenish minerals and micronutrients to prevent suboptimal health and adverse pregnancy and developmental outcomes. However, we are still falling short in our efforts to prevent hidden hunger and improve the nutritional status of women and children, thus new strategies are urgently needed. We are testing novel interventions to improve mineral and micronutrient status in women. These studies are part of our larger goals to improve maternal-child nutrition and our understanding of the mechanisms that contribute to nutrient transport, absorption and metabolism.
We are also evaluating programmes that aim to improve nutrition knowledge and reduce iron deficiency and anaemia (ID/IDA) in women, and are engaging with stakeholders from communities through to national governments and NGOs to better understand the people, health systems, and environments that influence hidden hunger and its treatment. These efforts are part of our goal to co-design frameworks for improved treatment and prevention of ID and IDA across the lifecycle.
-

THRIVE: a lifecycle health promotion and knowledge mobilisation tool to advance health literacy, health communication, and health span
Although the Developmental Origins of Health and Disease (DOHaD) recognises the importance of early exposures in the development of chronic conditions, our ability to harness this knowledge before irreversible processes affect health trajectories remains limited. Using machine learning approaches we are making a comprehensive catalogue of early influential risk and protective factors across social, environmental and biomedical fields, and developing a model for precise and personalised lifecycle health information. These studies are part of our larger goal to instrumentalise our understanding of DOHaD and develop a tool to identify resilience and risk trajectories to optimise health decision making and interventions. Learn more of this work with the THRIVE Change Lab.
-

Library of experience to inform lifecycle health research and care
Clinical and scientific evidence can only get us so far in understanding and improving lifecycle health trajectories. Stories, perspectives, and insights from experts-by-experience (EbE) are key pieces of evidence that can: 1. advance health research, care and policies for preconception, prenatal and postnatal health; 2. inspire dialogue to support health decision-making; 3. be a resource for advocacy. Integrating this evidence from experience with clinical and scientific evidence can ensure that research, care and health policies are designed with, and acceptable to, the community of EbEs these efforts are meant to serve. We are undertaking research to catalogue the efforts that are occurring in Canada and globally related to capturing the voices of EbE from preconception through the first 1000 days of life. We aim to understand how these experiences are captured and used to inform research, care and advocacy, and the challenges and opportunities that exist to equitably inform health literacy, care and policy for diverse populations. These efforts are part of our larger work with the THRIVE Change Lab to develop a library of lived/living experiences related to lifecycle health that serves as a virtual knowledge space to advance research, care, policy and advocacy in the developmental origins of health and disease.
-

Early investments, lasting impact
It is well known that there are major health gaps between men and women, largely driven by a lack of knowledge into the biology of women’s health and disease, and other social, environmental, and systemic factors that differentially affect genders and influence health outcomes. Critically, these health gaps also affect future generations. We believe closing the gap in funding for women’s health and health research will improve health outcomes for women and their children, and likely provide the best return on investment for governments seeking to make an impact in preventing, diagnosing and treating health conditions. We are capturing data on health funding, interventions, and outcomes, to better understand health gaps and opportunities to close these. This work is part of our larger advocacy efforts for improving women’s and lifecycle health, and is done in collaboration with Dr. Tim Regnault at Western University.
-

Postnatal nutrition and infant development following HIV exposure in utero
Rates of HIV transmission from mother to child are decreasing. Whether there is a lasting impact of maternal HIV infection on the development of the HIV negative infant remains to be explored. Further, little is known about the impact of pre- and postnatal nutritional environments on the growth, development and health of the HIV exposed but uninfected infant. We are investigating nutritional environments and infant growth in the context of HIV. Our work includes engaging with stakeholders to better understand the environments that shape health outcomes in mothers and infants affected by HIV, and studies investigating how maternal HIV infection alters the composition of nutrients, immune molecules and bioactive metabolites in breast milk, and if maternal HIV status, breastfeeding practices, and factors present in breast milk are associated with infant growth and health. These studies are part of our larger goal to improve the lifelong immune and metabolic function in HIV exposed infants.
Participate
If you want to go far, go together.
Our research spans disciplines from maternal health, fetoplacental and pregnancy physiology, child development and nutritional sciences, to biomedical sciences, molecular and systems biology, and microbiome sciences, to quantitative survey design and analysis and programme evaluation, to biostatistics, bioinformatics, and epidemiology. We integrate methods and techniques across these disciplines through our use of animal and cell culture models, human cohorts and large datasets.
We are always looking for great people.
Due to our collaborative and transdisciplinary approach, the Connor Lab seeks talented individuals with expertise in health and nutritional sciences, biomedical sciences, and data sciences. We provide the mentorship, facilities, and collaborative and networking opportunities for success in each team member's research project, and tailored to their career plans. Check out some of the exciting questions we are investigating. We encourage you to drop us a line if you want to join in. Send us a statement of your research interests and how you think our lab can help you achieve your professional goals, and a CV highlighting your relevant skills.
In this lab we commit to:
Equity: we commit to providing the mentorship, resources, knowledge, voice and opportunities people need to grow and succeed, and tailor these to each person’s place and goals. We also commit to privileging underrepresented groups and those whose power and agency has been diminished or taken, in our delivery of these supports.
Diversity: we seek diverse teammates, collaborators and opportunities to ensure that diverse perspectives, experiences, and approaches guide our work and reframe the questions we ask. We work to be both an ally and advocate for others, including those who may not hold power, privilege, and experience.
Inclusivity: we ask questions and behave respectfully, to ensure inclusion is possible for everyone on our team and with whom we work, and ideas and opinions can be shared, even if we don’t all agree.
Identity: we recognise identity is both shared and personal, and strive to learn about and support people’s stories and identity of themselves.
We recognise these commitments take consistent learning, asking questions, being open to growth and development when we are wrong, and working in service of and empowering others. We commit to exploring and reviewing our own positionality, power, and understanding of the world and others, to better support those we lead, teach, and mentor, and the research we do.
Dr. Connor also commits to:
Advocating for capacity building across the career lifecycle of scholars of equity-deserving and underrepresented groups.
Advancing knowledge and promoting scientific and scholarly advances in Canada and globally on under-researched groups and fields.
Advising governments, NGOs and Canadians across sectors on the value of fundamental and translational science and women’s and children’s health for scaled investments and (inter)national impact.
Meet the Team
Dr. Kristin Connor
Dr. Kristin Connor is an Associate Professor of Developmental Origins of Health and Disease in the Department of Health Sciences at Carleton University. She is passionate about improving and supporting maternal, fetal and child health. Her expertise lies in understanding how early life nutrition, including hidden hunger, and maternal health states influence maternal and pregnancy health, and shape the developmental and health trajectories of the fetus and child. Her research focuses on novel ways to predict individuals at-risk for adverse pregnancy outcomes, suboptimal development, and later chronic disease, and novel interventions to optimise maternal health and early developmental trajectories to reduce the incidence of adverse pregnancy outcomes, poor infant growth, and chronic diseases in later life.
Dr. Connor has expertise in convening, capacity building, and systems thinking for innovative problem-solving through her work in Canada and globally. She brings together academics, clinicians, policy influencers, people with lived/living experience, public health experts, NGOs, governments and enterprises for knowledge exchange and mobilisation to facilitate action and create value.
Amongst other roles, she is Vice-Chair of the Advisory Board for the Canadian Institutes of Health Research Institute for Human Development, Child and Youth Health; co-President of the Canadian Society for the Developmental Origins of Health and Disease; Councillor for the Society for Reproductive Investigation; co-founder of the Alliance Against Iron Deficiency and the THRIVE Change Lab; served as Associate Editor for the Journal of Developmental Origins of Health and Disease for nearly eight years; and has completed the Corporate Governance programme at the Wharton Business School.
-

Adaeze Ikechukwu
Adaeze has a background in Health Sciences, focusing on disability and chronic illness. She is particularly passionate about improving women's and children's health and nutrition—starting from early life—to help prevent conditions that can lead to long-term disability or chronic illness. Adaeze’s research uses data from a randomised controlled trial for the potential treatment of iron deficiency in reproductive aged women. She aims to better understand iron deficiency and treatment response through an exploration of dietary and sociodemographic influences.
-

Adel Yasin
Adel is a recent Honours BHSc graduate with a research background in epidemiology and statistics. His current research aims to understand the mechanisms linking early environments with neural tube defect risk and suboptimal fetoplacental development. His work uses placental metabolomics and transcriptomics to investigate how maternal-fetal-environment interactions shape early developmental outcomes.
-

Chloë Hayes
Chloë is a journalism student with a concentration in health sciences. She aspires to use journalism to effectively communicate new developments in health science research and public health to everyday people. She is particularly interested in women's health. She aims to investigate and report on the intersectional relationships between biology, identity, social structures, and the environment, and their impacts on maternal health, child development, and chronic disease risk. Her capstone research in the lab will introduce her to clinical trial research and better understand receptivity and acceptability of probiotics for women’s health.
-

Emma Chisholm
Emma’s background is in global health, specifically contraceptives through allied health services, focusing on how rurality can adversely impact health outcomes. She is interested in advancing women’s health and gender equity, as well as health literacy and knowledge translation - areas she considers essential for advancing equity and empowering traditionally marginalised communities. Emma’s research contributes to the prevention and treatment of iron deficiency (ID) in West Africa, focusing on empowering and engaging youth as local champions and knowledge brokers to promote health literacy on ID through co-designed knowledge mobilisation efforts. Her goal is to ultimately support evidence-based, community-informed policy and practice.
-

Erikles Barbosa
Erikles' background is in experimental pathology. His current research uses animal models to better understand the pathogenesis of neural tube defects and their comorbidities. He is particularly interested in how nutritional interventions, including prebiotics, probiotics, and micronutrients, can influence placental development and fetal health, and how the maternal gut microbiome may be key for shaping early environments important for the developing embryo/fetus and placenta. Erikles hopes his work will contribute to healthier pregnancies and ensure optimal development for future generations.
-
Hailey Scott
Hailey’s background is in pregnancy complications and placental development, with a particular focus on preterm birth and maternal underweight and obesity. Her research aims to understand placental maldevelopment and dysfunction in response to adverse early life environments. She is also interested in understanding the impact of early interventions to improve maternal, pregnancy and child health, including interventions to address nutritional deficiencies in reproductive aged women. She plays a key role in research coordination and direction in the lab.
-

Hauna Sheyholislami
Hauna’s background is in health sciences and bioinformatics. Her research focuses on the role of the gut microbiome and novel interventions in the health of reproductive aged and pregnant women and their infants. She is particularly interested in how the maternal gut microbiome and metabolome are altered in complex pregnancies. She is also exploring how a micronutrient intervention may alter the gut microbiome and metabolome in reproductive aged women.
-

Kieran Anderson-Barwin
Kieran is a new Registered Dietitian with an academic background in biomedical science and nutrition (BSc, BFNSc). With experience in medical administration, Kieran is passionate about healthcare, especially improving healthspan and enhancing quality of life throughout ageing. His commitment to evidence-based practices and promoting overall well-being defines his approach to health and nutrition. He is currently working on a clinical trial testing a novel intervention for the potential treatment of iron deficiency.
-

Lucas Carvalho Cardoso
Lucas’ interest is to study the effects of maternal nutrition on fetal development and how changes in the intrauterine environment affect adult health. His research attempts to understand the changes that malnutrition, associated with an episode of infection, can cause during pregnancy, focusing on relationships between the maternal/offspring guts, placenta, and fetal development.
-

Madeline Choy
Madeline’s research investigates evidence for ‘libraries of lived experience’ at a global scale, grounded in the DOHaD framework. She aims to identify libraries that capture voices of experts-by-experience related to pre-conception, perinatal, and maternal health. She is interested in analysing the gaps and opportunities to inform pregnancy-related health risks/benefits through an intersectional approach.
-

Melissa Watton
Melissa’s research focuses on how maternal metabolites influence fetal growth and development, particularly the developing brain. She is specifically interested in the placenta-fetal brain axis and which influential metabolites and pathways may contribute to altered developmental trajectories, including of the developing brain. She also aspires to connect her research to testing future therapeutics that can optimise maternal health and prevent adverse health trajectories in offspring.
Recent grad!
-

Miguel Massiris
Miguel's research investigates, develops, and tests automatic and semi-automatic knowledge graph text models based on medical research. He aims to create virtual assistants for use in neonatal and paediatric clinics, where relevant information can be accessed by and shared with medical professionals and other stakeholders. These assistants can help to establish communication channels and disseminate information amongst various stakeholders, ultimately for more informed and shared health decision-making. Miguel is undertaking his PhD in Engineering through Universidad Nacional del Sur, Argentina, and is co-supervised by Dr. Kristin Connor and Dr. Claudio Delrieux from the Department of Electrical and Computer Engineering, Universidad Nacional del Sur.
-

Olivia Wilding-Davies
Olivia’s background is interdisciplinary health science, including social and early life determinants of health. As a Zimbabwean with interest and expertise in global health, Olivia’s research aims to understand the individual, community, and external factors that influence success of community-based interventions for the prevention and treatment of iron deficiency in West Africa. Ultimately, her goal is to inform intervention design and provide evidence for adapting and scaling interventions that tackle hidden hunger to suit local and population needs.
-

Sadra Mohammadkhani
Sadra’s research investigates the impact of maternal obesity and episodes of viral infection on pregnancy and offspring development. He is particularly interested in changes at the maternal-fetal interface and placental pathways involved in poor pregnancy outcomes. He is also an aspiring pharmaceutical researcher, specifically in the field of drug development for diseases related to prions.
-
Thaina Ferraz
Thaina’s research focuses on how maternal obesity and episodes of viral infection during pregnancy may create an opportunity for poor pregnancy health and offspring development via changes at the maternal-fetal interface. She is particularly interested in placental genes/pathways associated with nutrient transport and inflammatory response and fetal/offspring growth and postnatal inflammatory phenotype. She is also investigating whether a microbe-based intervention to the mother during critical windows of fetoplacental development may correct poor gestational tissue development and function and optimise fetal growth.
-

Zahra van Gaalen
Zahra’s research focuses on women’s health equity, policy, and implementation science. Her work examines how policies and programmes shape equitable nutrition interventions for women and girls in West Africa, with a focus on addressing iron deficiency and anaemia. She aims to identify policy gaps and foster collaboration to guide scalable, sustainable interventions that strengthen women’s agency in health and nutrition.
Collaborations
Dr. Tim Van Mieghem, Department of Obstetrics and Gynaecology, Sinai Health System, Toronto
With Dr. Van Mieghem, we are investigating the role of the gut microbiome in the pathogenesis of fetal spina bifida and testing novel interventions for the prevention of this condition. We are grateful to be supported by the Canadian Institutes of Health Research (CIHR) for this work.
Dr. Enrrico Bloise, Department of Morphology, Instituto De Ciencias Biologicas, Universidade Federal De Minas Gerais, Brazil
With Dr. Bloise and his team, we are investigating how maternal underweight and obesity impact gut and placental transport systems in an animal model, and impact intrauterine tissue function and defence and risk for preterm labour in a human cohort. We are grateful to have the this work supported by the National Sciences and Engineering Research Council of Canada (NSERC) and an International Research Seed Grant through Carleton University’s Research and International office.
Dr. David Grynspan (Vernon Jubilee Hospital and University of British Columbia)
Our team works closely with Dr. Grynspan on studies to better understand placental pathologies and placental development. We are grateful to be supported by the Molly Towell Perinatal Research Foundation, CIHR, and the Faculty of Science at Carleton University for this work.
THRIVE: Sandra T. Davidge (U Edmonton, Edmonton), Claudio Delrieux (Universidad Nacional del Sur Argentina), Daniel Goldowitz (UBC, Vancouver), Pablo Nepomnaschy (Simon Fraser U, Vancouver), Ashley Wazana (McGill U, Montreal)
With the THRIVE (Towards Human Resiliency In Varying Environments) team, we are developing a tool to identify resilience and risk trajectories to optimise health decision making and interventions. We are grateful for support from CIHR to seed the foundational work. Learn more about the THRIVE Change Lab.
LIFe and Dr. Bénédicte Fontain-Bisson (U Ottawa)
With Dr. Fontain-Bisson, we are testing novel interventions developed by Lucky Iron Fish Enterprises to tackle the hidden hunger of iron deficiency. We are grateful to be supported by LIFe in these efforts.
Ontario Birth Study, Drs. Alan Bocking, Stephen Lye, Cynthia Maxwell
Through the Ontario Birth Study, we aim to understand the role of the microbiome in shaping metabolic health and disease trajectories in mothers and their offspring. To do this we have developed the MATaDOR (Microbial Approaches Targeting Diabetes and Obesity Risk) Early Life Study. We are grateful to have this work supported by the Garfield Westin Foundation and the Canadian Foundation for Women’s Health, and the McLaughlin Centre at the University of Toronto.
MIREC Cohort, Dr. Tye Arbuckle
We are collaborating with a team of investigators across Canada through the Maternal-Infant Research on Environmental Chemicals (MIREC) cohort to understand the relationships between maternal weight before and during pregnancy, and heavy metal exposure, on infant cognitive outcomes. We are also interested in determining whether the early life nutritional environment modifies these relationships. We are grateful to have this work supported by the Faculty of Science at Carleton University.
Past Connor Lab Members
-
PDF & Research Associates
Dr. Jessie Burns
Dr. Samantha Benton
Dr. Constance Nana
-
PhD
Dr. Marina White
Dr. Lilian Martinelli (Co-supervisor; PhD Cell Biology, Federal University of Minas Gerais, Brazil).
-
MSc Health Sciences
Clara Miller
Hailey Scott
-
MSc Health: Science, Technology & Policy
Alissa Vaziri
Devyn Hoopfer
Ayshia Bailie
Aleyna Akgun
Hauna Sheyholislami
Ayah Abdul-Hussei
Ayesha Kareem
Shrankhala Tewari
Jamie Strain
Zoe West
Iryna Demchenko
Lee Clark
Morgan Belsek
Queena Chen
Jenna Coles
Makenzie Weekes
-
Undergraduate Researchers
Carolyn McCleary
Zahra Mashhadi
Madeline Choy
Romika Subedi
Emily Barmania
Melissa Watton
Jayden Arif-Pardy
Hasan Abdo
Oluwatomike Aribaloye
Israa Zareef
Eleanor Duffley
Christopher Roche
Elia Palladino
Sebastian Srugo
James Bilyk
Madison Donoghue
Claudia Sendanyoye
-
Visiting international student researchers
Juliette Robert, MSc, Pharmacology and Biology, Polytech Nice Sophia – Université Côte d’Azur. Supported through Université Côte d’Azur.
Odara Champoudry da Silva, BScH, Department of Physiological Sciences, Federal University of Maranhão (UFMA), Brazil. Supported through the Emerging Leaders in the Americas Programme.
Tiffany Kerdiles, MSc, Pharmacology and Biotechnology, Polytech Nice Sophia – Université Côte d’Azur. Supported through Université Côte d’Azur.
Michael Daly, PhD, University of Bristol. Supported through a UKRI-Mitacs Globalink UK-Canada Doctoral Exchange Award.
References
1. Gotay et al. (2013) Updating the Canadian obesity maps: An epidemic in progress. Canadian Journal of Public Health 104:e64-e68
2. WHO (2013) http://www.who.int/dietphysicalactivity/childhood/en/
3. Institute for Health Metrics and Evaluation (IHME) (2013) GBD Cause Patterns. IHME, University of Washington, Seattle
4. NCD Risk Factor Collaboration (2016) Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet 387:1377–1396
5. Tarasuk et al. (2014). Household food insecurity in Canada, 2012. Toronto: Research to identify policy options to reduce food insecurity (PROOF). Retrieved from http://nutritionalsciences.lamp.utoronto.ca/
6. Black et al. (2013) Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 382:427–451
7. Black et al. (2008) Maternal and child undernutrition: global and regional exposures and health consequences. Lancet 371:243–260
8. Han et al. (2011) Maternal underweight and the risk of preterm birth and low birth weight: a systematic review and meta-analyses. International Journal of Epidemiology 40:65-101
9. Cnattingius et al. (2009) Maternal obesity and risk of preterm delivery. JAMA 309:2362-2370
10. Challis et al. (2009) Inflammation and pregnancy. Reproductive Sciences 16:206-215
11. Goldenberg et al. (2008) Epidemiology and causes of preterm birth. Lancet 371:75-84
12. Canadian Institute for Health Information (CIHI) (2006). Giving birth in Canada: The costs. CIHI, Ottawa
13. Canadian Institute for Health Information (CIHI) & Public Health Agency of Canada (PHAC) (2011) Obesity in Canada: A joint report from PHAC and CIHI, Ottawa
14. Kendall et al. (2010) Investing in Prevention: Improving health and creating sustainability: the Provincial Health Officer’s special report. Office of the Provincial Health Officer/British Columbia, September 2010. Downloaded October 2011 from www.health.gov.bc.ca/library/publications/year/2010/Investing_in_prevention_improving_health_and_creating_sustainability.pdf
15. Canadian Public Health Association (2016) Making the Economic Case for Investing in Public Health and the social determinants of health. Accessed July 10, 2016 from http://www.cpha.ca/en/programs/social-determinants/frontlinehealth/economics.aspx#f5